The Palliative Care and Nursing Ethics Hub
Contributing to excellence in palliative care and nursing ethics nationally and internationally
A Research Hub of the Centre for Research on Health and Nursing, in partnership with the University of Ottawa and the Canadian Nurses Association
What’s new?

February Workshop: Designing a Palliative Care Course
This February we will be hosting a workshop to plan an undergraduate nursing curriculum on a palliative approach to care. Join us virtually at 12:30pm EST on February 3rd, 2026.
Sign up via the Join Us tab to receive more details about this and future events.
Highlights
Statement on the Killing of Alex Pretti
Hub mentors, David Wright, Kim McMillan, Christine McPherson, and Marianne Sofronas, share a statement on the killing of Alex Pretti.
The Spectrum of Grief in Nursing: A Panel Discussion
Hub professors Kim McMillan and David Wright contributed to this panel discussion about grief in nursing, which received over 500 registrations! They were interviewed together and spoke about navigating the intersections of personal and professional loss.
LGBTQ+ stories of death-related grief: A narrative inquiry
We are recruiting for a study on LGBTQ+ stories of death-related grief. This work is funded by the Social Sciences and Humanities Research Council.
CPCNA Annual Awards
At this year’s annual lecture, the CPCNA continued its tradition of recognizing outstanding nurses for their exceptional contributions to the community and the field of palliative care.
We are thrilled to congratulate Dr. Coby Tschanz, recipient of the Lifetime Achievement Award, and Dr. Val Fiset, recipient of the Leadership Award. Their dedication, leadership, and impact continue to shape and strengthen palliative nursing in Canada.
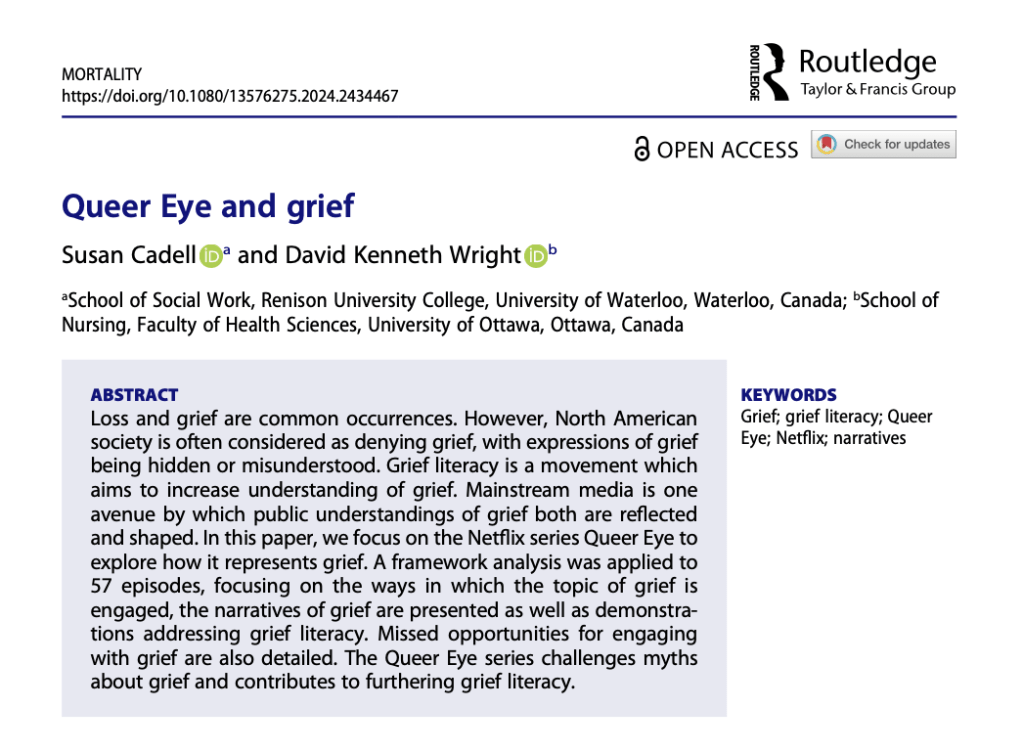
New publication: Queer Eye & grief
Dr. Susan Cadell, and hub lead, Dr. David Kenneth Wright, have just published a new article.
Proudly powered by WordPress